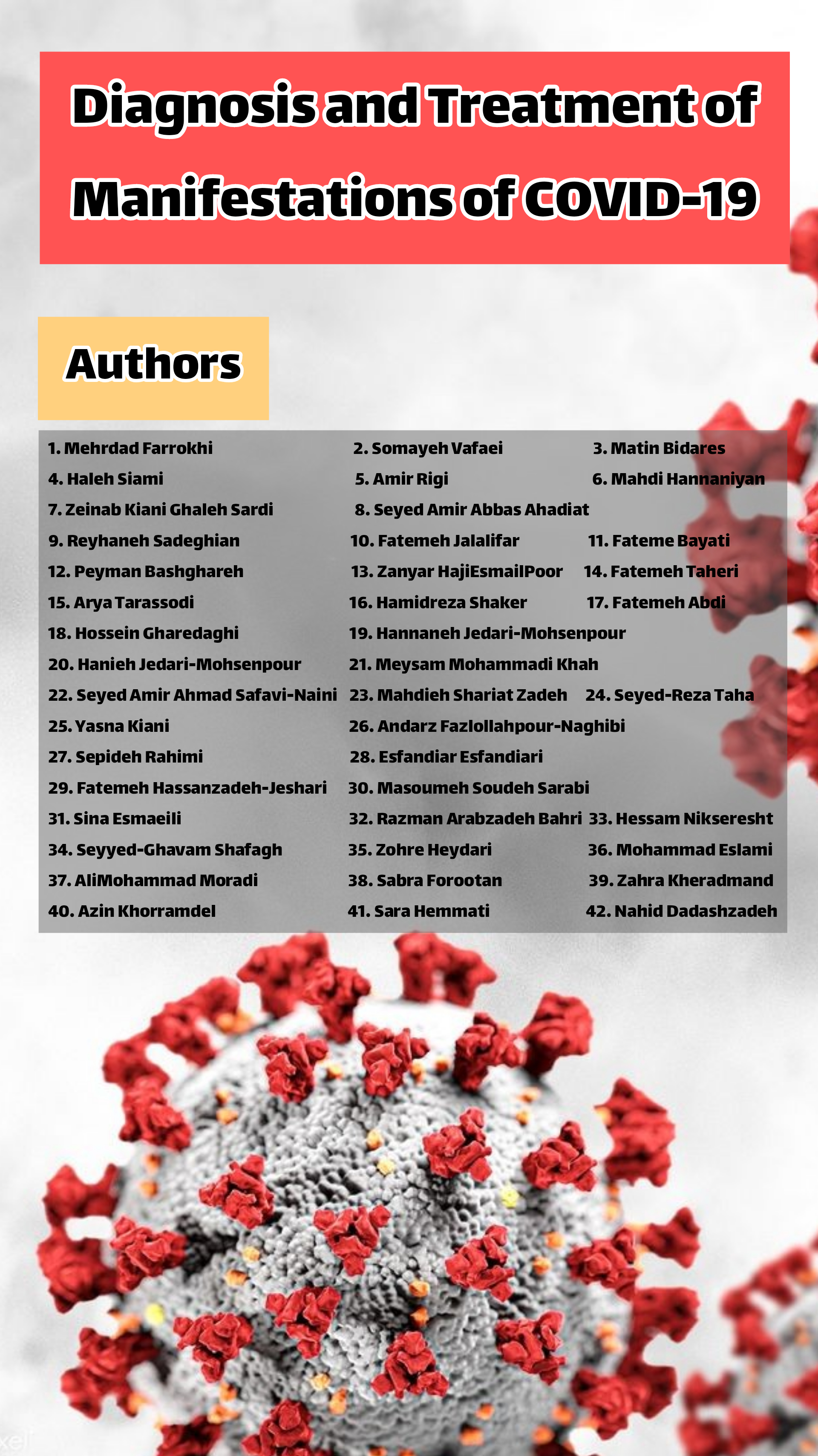
Academic Textbook: Diagnosis and Treatment of Manifestations of COVID-19
Keywords:
Diagnosis , Treatment , Manifestations , COVID-19Abstract
The diagnosis and treatment of manifestations of COVID-19 have evolved significantly since the onset of the pandemic. With an expanding understanding of the virus and its impact on the human body, healthcare professionals have refined their approaches to effectively diagnose and manage the disease. Diagnosis primarily relies on testing for the presence of the SARS-CoV-2 virus, typically through RT-PCR tests, antigen tests, or serological assays. Early in the pandemic, diagnosis centered on identifying common symptoms such as fever, cough, and shortness of breath. However, as our knowledge has grown, we've come to recognize a broader spectrum of manifestations, including loss of taste or smell, gastrointestinal issues, and neurological symptoms. Once diagnosed, the treatment of COVID-19 focuses on managing symptoms, preventing complications, and reducing viral spread. Mild cases often require only supportive care, such as rest, hydration, and over-the-counter medications to alleviate fever and pain. In moderate to severe cases, especially those involving respiratory distress, hospitalization may be necessary. In these instances, oxygen therapy, antiviral medications like remdesivir, corticosteroids to reduce inflammation, and in some cases, immune-modulating drugs are employed. The emergence of vaccines has also revolutionized the approach to COVID-19 treatment, shifting the focus towards prevention. Vaccination campaigns aim to reduce the severity of the disease, decrease hospitalizations, and ultimately achieve herd immunity. Furthermore, ongoing research continues to explore novel treatments, including monoclonal antibodies, immunomodulators, and repurposed drugs, with the goal of improving outcomes and reducing mortality rates.
References
Clelland CL, Ramiah K, Steinberg L, Clelland JD. Analysis of the impact of antidepressants and other medications on COVID-19 infection risk in a chronic psychiatric in-patient cohort. BJPsych open. 2021;8(1):e6.
Elhassan M, Ahmad H, Mohamed M, Saidahmed O, Elhassan AE. From Muscles to Wires: Report of Two Cases and Literature Review on COVID-19 Vaccination and Cardiac Conduction Disturbance. Cureus. 2021;13(10):e18805.
Muhammad A, Iftikhar N, Mashhood A, Virdi G, Ud Din H, Akbar A, et al. Dermatological Manifestations of COVID-19 in Patients Reporting to a Tertiary Care Hospital in Rawalpindi, Pakistan. Cureus. 2021;13(10):e18973.
Zarubova J, Zhang X, Hoffman T, Hasani-Sadrabadi MM, Li S. Biomaterial-based immunoengineering to fight COVID-19 and infectious diseases. Matter. 2021;4(5):1528-54.
El-Anwar MW, Elzayat S, Fouad YA. ENT manifestation in COVID-19 patients. Auris, nasus, larynx. 2020;47(4):559-64.
Zhang H, Shao B, Dang Q, Chen Z, Zhou Q, Luo H, et al. Pathogenesis and Mechanism of Gastrointestinal Infection With COVID-19. Frontiers in immunology. 2021;12:674074.
Aslan AT, Şimşek H. Clinical Features and Pathophysiological Mechanisms of COVID-19-associated Gastrointestinal Manifestations. Euroasian journal of hepato-gastroenterology. 2021;11(2):81-6.
Gulen M, Satar S. Uncommon presentation of COVID-19: Gastrointestinal bleeding. Clinics and Research in Hepatology and Gastroenterology. 2020;44(4):e72-e6.
Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology. 2020;158(6):1518-9.
Kotfis K, Skonieczna-Żydecka K. COVID-19: gastrointestinal symptoms and potential sources of SARS-CoV-2 transmission. Anaesthesiology intensive therapy. 2020;52(2):171.
Silva FAFd, Brito BBd, Santos MLC, Marques HS, Silva RTd, Carvalho LSd, et al. COVID-19 gastrointestinal manifestations: a systematic review. Revista da Sociedade Brasileira de Medicina Tropical. 2020;53.
Yang L, Tu L. Implications of gastrointestinal manifestations of COVID-19. The Lancet Gastroenterology & Hepatology. 2020;5(7):629-30.
Ashcroft J, Hudson V, Davies R. COVID-19 gastrointestinal symptoms mimicking surgical presentations. Annals of Medicine and Surgery. 2020;56:108.
Kopel J, Perisetti A, Gajendran M, Boregowda U, Goyal H. Clinical insights into the gastrointestinal manifestations of COVID-19. Digestive diseases and sciences. 2020;65:1932-9.
Du M, Cai G, Chen F, Christiani DC, Zhang Z, Wang M. Multiomics evaluation of gastrointestinal and other clinical characteristics of COVID-19. Gastroenterology. 2020;158(8):2298-301. e7.
Schmulson M, Dávalos M, Berumen J. Beware: Gastrointestinal symptoms can be a manifestation of COVID-19. Revista de Gastroenterología de México (English Edition). 2020;85(3):282-7.
Jimenez DG, Rodríguez-Belvís MV, Gonzalez PF, Ortega GD, Segarra O, Benitez EM, et al. COVID-19 gastrointestinal manifestations are independent predictors of PICU admission in hospitalized pediatric patients. The Pediatric infectious disease journal. 2020;39(12):e459-e62.
Tian Y, Rong L, Nian W, He Y. gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Alimentary pharmacology & therapeutics. 2020;51(9):843-51.
Kaźmierczak-Siedlecka K, Vitale E, Makarewicz W. COVID-19-gastrointestinal and gut microbiota-related aspects. Eur Rev Med Pharmacol Sci. 2020;24(20):10853-9.
Tullie L, Ford K, Bisharat M, Watson T, Thakkar H, Mullassery D, et al. Gastrointestinal features in children with COVID-19: an observation of varied presentation in eight children. The Lancet Child & Adolescent Health. 2020;4(7):e19-e20.
Gralnek IM, Hassan C, Beilenhoff U, Antonelli G, Ebigbo A, Pellisè M, et al. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020;52(06):483-90.
Wong SH, Lui RN, Sung JJ. Covid‐19 and the digestive system. Journal of gastroenterology and hepatology. 2020;35(5):744-8.
Galanopoulos M, Gkeros F, Doukatas A, Karianakis G, Pontas C, Tsoukalas N, et al. COVID-19 pandemic: Pathophysiology and manifestations from the gastrointestinal tract. World journal of gastroenterology. 2020;26(31):4579.
Sinonquel P, Roelandt P, Demedts I, Van Gerven L, Vandenbriele C, Wilmer A, et al. COVID‐19 and gastrointestinal endoscopy: what should be taken into account? Digestive Endoscopy. 2020;32(5):723-31.
Ye Q, Wang B, Zhang T, Xu J, Shang S. The mechanism and treatment of gastrointestinal symptoms in patients with COVID-19. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2020;319(2):G245-G52.
Rokkas T. Gastrointestinal involvement in COVID-19: a systematic review and meta-analysis. Annals of gastroenterology. 2020;33(4):355.
Zhou Z, Zhao N, Shu Y, Han S, Chen B, Shu X. Effect of gastrointestinal symptoms in patients with COVID-19. Gastroenterology. 2020;158(8):2294.
Cheong J, Bartell N, Peeraphatdit T, Mosli M, Al-Judaibi B. Gastrointestinal and liver manifestations of COVID-19. Saudi journal of gastroenterology: official journal of the Saudi Gastroenterology Association. 2020;26(5):226.
Zhang M, Zhou Y, Li H, Peng Y, Qiu P, Shi X, et al. COVID-19: gastrointestinal symptoms from the view of gut–lung axis. European Journal of Gastroenterology & Hepatology. 2021;33(5):610-2.
Ouali SE, Achkar J-P, Lashner B, Regueiro M. Gastrointestinal manifestations of COVID-19. Cleveland Clinic Journal of Medicine. 2020.
Zhao Y, Cao Y, Wang S, Cai K, Xu K. COVID‐19 and gastrointestinal symptoms. The British Journal of Surgery. 2020.
Hunt RH, East JE, Lanas A, Malfertheiner P, Satsangi J, Scarpignato C, et al. COVID-19 and Gastrointestinal Disease: Implications for the Gastroenterologist. Digestive Diseases. 2021;39(2):119-39.
Xu Y, Liu P, Gu J. Gastrointestinal and liver involvement in patients with COVID-19. The Lancet Gastroenterology & Hepatology. 2020;5(9):798-9.
Smyk W, Janik MK, Portincasa P, Milkiewicz P, Lammert F, Krawczyk M. COVID‐19: focus on the lungs but do not forget the gastrointestinal tract. European journal of clinical investigation. 2020;50(9):e13276.
Zhang J, Garrett S, Sun J. Gastrointestinal symptoms, pathophysiology, and treatment in COVID-19. Genes & diseases. 2021;8(4):385-400.
Dahiya DS, Kichloo A, Albosta M, Pagad S, Wani F. Gastrointestinal implications in COVID-19. Journal of Investigative Medicine. 2020;68(8):1397-401.
Agarwal A, Chen A, Ravindran N, To C, Thuluvath PJ. Gastrointestinal and liver manifestations of COVID-19. Journal of clinical and experimental hepatology. 2020;10(3):263-5.
Patel KP, Patel PA, Vunnam RR, Hewlett AT, Jain R, Jing R, et al. Gastrointestinal, hepatobiliary, and pancreatic manifestations of COVID-19. Journal of Clinical Virology. 2020;128:104386.
Aguila EJT, Cua IHY, Fontanilla JAC, Yabut VLM, Causing MFP. Gastrointestinal manifestations of COVID‐19: impact on nutrition practices. Nutrition in Clinical Practice. 2020;35(5):800-5.
Perisetti A, Goyal H, Gajendran M, Boregowda U, Mann R, Sharma N. Prevalence, mechanisms, and implications of gastrointestinal symptoms in COVID-19. Frontiers in medicine. 2020;7:741.
Mandal A, Konala VM, Adapa S, Naramala S, Gayam V. Gastrointestinal manifestations in COVID-19 infection and its practical applications. Cureus. 2020;12(6).
Mao R, Qiu Y, He J-S, Tan J-Y, Li X-H, Liang J, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. The lancet Gastroenterology & hepatology. 2020;5(7):667-78.
Kariyawasam JC, Jayarajah U, Riza R, Abeysuriya V, Seneviratne SL. Gastrointestinal manifestations in COVID-19. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2021.
Ai J-W, Zi H, Wang Y, Huang Q, Wang N, Li L-Y, et al. Clinical characteristics of COVID-19 patients with gastrointestinal symptoms: an analysis of seven patients in China. Frontiers in medicine. 2020;7:308.
Alboraie M, Piscoya A, Tran QT, Mendelsohn RB, Butt AS, Lenz L, et al. The global impact of COVID-19 on gastrointestinal endoscopy units: An international survey of endoscopists. Arab Journal of Gastroenterology. 2020;21(3):156-61.
Nie K, Yang Y-Y, Deng M-Z, Wang X-Y. Gastrointestinal insights during the COVID-19 epidemic. World journal of clinical cases. 2020;8(18):3934.
Zhang H, Liao Y-S, Gong J, Liu J, Xia X, Zhang H. Clinical characteristics of coronavirus disease (COVID-19) patients with gastrointestinal symptoms: A report of 164 cases. Digestive and Liver Disease. 2020;52(10):1076-9.
Switzer B, Haanen J, Lorigan PC, Puzanov I, Turajlic S. Clinical and immunologic implications of COVID-19 in patients with melanoma and renal cell carcinoma receiving immune checkpoint inhibitors. Journal for immunotherapy of cancer. 2021;9(7).
Touyz RM, Boyd MOE, Guzik T, Padmanabhan S, McCallum L, Delles C, et al. Cardiovascular and Renal Risk Factors and Complications Associated With COVID-19. CJC open. 2021;3(10):1257-72.
Bitencourt L, Pedrosa AL, de Brito S, Fróes ACF, de Carvalho ST, Fonseca GG, et al. COVID-19 and Renal Diseases: An Update. Current drug targets. 2021;22(1):52-67.
Rigual R, Ruiz-Ares G, Rodriguez-Pardo J, Fernández-Prieto A, Navia P, Novo JR, et al. Concurrent Cerebral, Splenic, and Renal Infarction in a Patient With COVID-19 Infection. The neurologist. 2021.
Belfort DSP, Marcondes-Braga FG, Mangini S, Cafezeiro CRF, Furlan DAG, Bacal F. Aortic and Renal Artery Thrombosis as the First Clinical Manifestation of COVID-19 in a Heart Transplant Recipient. Arquivos brasileiros de cardiologia. 2021;117(5):1045-7.
Takamatsu C, Devis P, Tolouian R. COVID-19 and renal infarct: To be or not to be on anticoagulation. Clinical nephrology Case studies. 2021;9:117-22.
Choe PG, Jeong SI, Kang CK, Yang L, Lee S, Cho JY, et al. Exploration for the effect of renal function and renal replacement therapy on pharmacokinetics of remdesivir and GS-441524 in patients with COVID-19: A limited case series. Clinical and translational science. 2021.
Rezq S, Huffman AM, Basnet J, Yanes Cardozo LL, Romero DG. Cardiac and Renal SARS-CoV-2 Viral Entry Protein Regulation by Androgens and Diet: Implications for Polycystic Ovary Syndrome and COVID-19. International journal of molecular sciences. 2021;22(18).
Banshodani M, Shintaku S, Kawanishi H. Combination therapy for COVID-19 in hemodialysis patients: Pharmacological treatments and renal replacement therapy based on the severity. Therapeutic apheresis and dialysis : official peer-reviewed journal of the International Society for Apheresis, the Japanese Society for Apheresis, the Japanese Society for Dialysis Therapy. 2021.
Ryan R, Taylor I, Laing C, Singer M, Gondongwe D, Maccallum N, et al. Comparison of renal replacement therapy and renal recovery before and during the COVID-19 pandemic: a single center observational study. Minerva anestesiologica. 2021;87(11):1209-16.
Lee AC, Li WT, Apostol L, Ma J, Taub PR, Chang EY, et al. Cardiovascular, cerebrovascular, and renal co-morbidities in COVID-19 patients: A systematic-review and meta-analysis. Computational and structural biotechnology journal. 2021;19:3755-64.
Medjeral-Thomas NR, Troldborg A, Hansen AG, Gisby J, Clarke CL, Prendecki M, et al. Plasma Lectin Pathway Complement Proteins in Patients With COVID-19 and Renal Disease. Frontiers in immunology. 2021;12:671052.
Bruno PF, Cappuccilli M, Spazzoli A, De Liberali M, Sejdiu B, Napoli M, et al. COVID-19 Infection: Viral Clearance and Antibody Response in Dialysis Patients and Renal Transplant Recipients. Nephron. 2021;145(4):363-70.
Eriksson KE, Campoccia-Jalde F, Rysz S, Rimes-Stigare C. Continuous renal replacement therapy in intensive care patients with COVID-19; survival and renal recovery. Journal of critical care. 2021;64:125-30.
Khoury EE, Knaney Y, Fokra A, Kinaneh S, Azzam Z, Heyman SN, et al. Pulmonary, cardiac and renal distribution of ACE2, furin, TMPRSS2 and ADAM17 in rats with heart failure: Potential implication for COVID-19 disease. Journal of cellular and molecular medicine. 2021;25(8):3840-55.
Sookaromdee P, Wiwanitkit V. Novel coronavirus infection (COVID-19) and renal failure: An observation from cases in the 1(st) month of outbreak. Saudi journal of kidney diseases and transplantation : an official publication of the Saudi Center for Organ Transplantation, Saudi Arabia. 2020;31(6):1455.
Arachchillage DRJ, Shi C, Saliu D, Kozman P, Mi E, Buti N, et al. Efficacy and Safety of D-dimer, Weight, and Renal Function-Adjusted Thromboprophylaxis in Patients with Coronavirus Disease 2019 (COVID-19). Seminars in thrombosis and hemostasis. 2021;47(4):436-41.
Elec AD, Oltean M, Goldis P, Cismaru C, Lupse M, Muntean A, et al. COVID-19 after kidney transplantation: Early outcomes and renal function following antiviral treatment. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2021;104:426-32.
Hittesdorf E, Panzer O, Wang D, Stevens JS, Hastie J, Jordan DA, et al. Mortality and renal outcomes of patients with severe COVID-19 treated in a provisional intensive care unit. Journal of critical care. 2021;62:172-5.
Doher MP, Torres de Carvalho FR, Scherer PF, Matsui TN, Ammirati AL, Caldin da Silva B, et al. Acute Kidney Injury and Renal Replacement Therapy in Critically Ill COVID-19 Patients: Risk Factors and Outcomes: A Single-Center Experience in Brazil. Blood purification. 2021;50(4-5):520-30.
Yang X, Tian S, Guo H. Acute kidney injury and renal replacement therapy in COVID-19 patients: A systematic review and meta-analysis. International immunopharmacology. 2021;90:107159.
Fominskiy EV, Scandroglio AM, Monti G, Calabrò MG, Landoni G, Dell'Acqua A, et al. Prevalence, Characteristics, Risk Factors, and Outcomes of Invasively Ventilated COVID-19 Patients with Acute Kidney Injury and Renal Replacement Therapy. Blood purification. 2021;50(1):102-9.
Adapa S, Chenna A, Balla M, Merugu GP, Koduri NM, Daggubati SR, et al. COVID-19 Pandemic Causing Acute Kidney Injury and Impact on Patients With Chronic Kidney Disease and Renal Transplantation. Journal of clinical medicine research. 2020;12(6):352-61.
Thomas T, Stefanoni D, Reisz JA, Nemkov T, Bertolone L, Francis RO, et al. COVID-19 infection results in alterations of the kynurenine pathway and fatty acid metabolism that correlate with IL-6 levels and renal status. medRxiv : the preprint server for health sciences. 2020.
Adapa S, Aeddula NR, Konala VM, Chenna A, Naramala S, Madhira BR, et al. COVID-19 and Renal Failure: Challenges in the Delivery of Renal Replacement Therapy. Journal of clinical medicine research. 2020;12(5):276-85.
Özkan Oktay E, Tuncay S, Kaman T, Karasakal Ö F, Özcan Ö, Soylamiş T, et al. An update comprehensive review on the status of COVID-19: vaccines, drugs, variants and neurological symptoms. Turkish journal of biology = Turk biyoloji dergisi. 2021;45(4):342-57.
Moore P, Esmail F, Qin S, Nand S, Berg S. Hypercoagulability of COVID-19 and Neurological Complications: A Review. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2021;31(1):106163.
Giacalone M, Tovani-Palone MR, Marin L, Febbi M, Russano T, Giacalone A. Neurological and neuropsychiatric disorders associated with COVID-19. Part I: overview and neurological disorders. Einstein (Sao Paulo, Brazil). 2021;19:eCE6448.
Veleri S. Neurotropism of SARS-CoV-2 and neurological diseases of the central nervous system in COVID-19 patients. Experimental brain research. 2021:1-17.
Liu L, Ni SY, Yan W, Lu QD, Zhao YM, Xu YY, et al. Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: A systematic review, meta-analysis and call for action. EClinicalMedicine. 2021;40:101111.
Aljomah L, Almedlej S, Baarmah D, Altwaijri W, Alrumayyan A, Alrifai MT, et al. Pediatrics COVID-19 and neurological manifestations: Single tertiary centre experience. eNeurologicalSci. 2021;24:100355.
Iftikhar S, Ghias M, Shahid S, Ali MR, Hassan MU, Numan A. Clinical and biochemical indicators of disease severity and neurological findings in COVID-19: A study of King Edward Medical University (KEMU), Pakistan. Pakistan journal of pharmaceutical sciences. 2021;34(1(Supplementary)):275-81.
Chu JY, Kaliwal Y, Koh M, Chen R, Chow CM, Ko DT, et al. COVID-19 and its Cardiac and Neurological Complications among Ontario Visible Minorities. The Canadian journal of neurological sciences Le journal canadien des sciences neurologiques. 2021:1-10.
Hess DC, Rutkowski E, Morgan J, McCluskey L. COVID-19 and neurological symptoms: is the SARS-CoV-2 virus neurotropic? Conditioning medicine. 2020;3(5):241-5.
Edison P. Brain Connectivity and Neurological Sequalae in COVID-19. Brain connectivity. 2021;11(5):331-2.
Davies DA, Adlimoghaddam A, Albensi BC. The Effect of COVID-19 on NF-κB and Neurological Manifestations of Disease. Mol Neurobiol. 2021;58(8):4178-87.
Kumar AA, Lee SWY, Lock C, Keong NC. Geographical Variations in Host Predisposition to COVID-19 Related Anosmia, Ageusia, and Neurological Syndromes. Frontiers in medicine. 2021;8:661359.
Mussa BM, Srivastava A, Verberne AJM. COVID-19 and Neurological Impairment: Hypothalamic Circuits and Beyond. Viruses. 2021;13(3).
Jakhmola S, Baral B, Muduli K, Suar M, Das P, Patnaik PK, et al. The interrelation of COVID-19 and neurological modalities. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2021;42(6):2157-60.
Sun B, Tang N, Peluso MJ, Iyer NS, Torres L, Donatelli JL, et al. Characterization and Biomarker Analyses of Post-COVID-19 Complications and Neurological Manifestations. Cells. 2021;10(2).
Soltani S, Tabibzadeh A, Zakeri A, Zakeri AM, Latifi T, Shabani M, et al. COVID-19 associated central nervous system manifestations, mental and neurological symptoms: a systematic review and meta-analysis. Reviews in the neurosciences. 2021;32(3):351-61.
Hosseini N, Nadjafi S, Ashtary B. Overview of COVID-19 and neurological complications. Reviews in the neurosciences. 2021;32(6):671-91.
Zirpe KG, Dixit S, Kulkarni AP, Sapra H, Kakkar G, Gupta R, et al. Pathophysiological Mechanisms and Neurological Manifestations in COVID-19. Indian journal of critical care medicine : peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2020;24(10):975-80.
Jensen-Kondering U, Neumann A, Margraf NG, Gövert F, Brüggemann N, Schunk D, et al. Cerebral Imaging in Patients with COVID-19 and Neurological Symptoms: First Experience from two University Hospitals in Northern Germany. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2021;193(6):667-71.
Assari S. COVID-19 Pandemic and Neurological Disease: A Critical Review of the Existing Literature. Hospital practices and research. 2020;5(3):81-6.
van der Meulen M, Kleineberg NN, Schreier DR, García-Azorin D, Di Lorenzo F. COVID-19 and neurological training in Europe: from early challenges to future perspectives. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2020;41(12):3377-9.
Acar T, Acar BA, Aras YG, Doğan T, Boncuk S, Eryılmaz HA, et al. Demographic characteristics and neurological comorbidity of patients with COVID-19. Revista da Associacao Medica Brasileira (1992). 2020;66Suppl 2(Suppl 2):82-5.
Ferini-Strambi L, Salsone M. COVID-19 and neurological disorders: are neurodegenerative or neuroimmunological diseases more vulnerable? J Neurol. 2021;268(2):409-19.
Ganapathy K. Telemedicine and Neurological Practice in the COVID-19 Era. Neurology India. 2020;68(3):555-9.
Hassanzadeh K, Perez Pena H, Dragotto J, Buccarello L, Iorio F, Pieraccini S, et al. Considerations around the SARS-CoV-2 Spike Protein with Particular Attention to COVID-19 Brain Infection and Neurological Symptoms. ACS chemical neuroscience. 2020;11(15):2361-9.
Beghi E, Feigin V, Caso V, Santalucia P, Logroscino G. COVID-19 Infection and Neurological Complications: Present Findings and Future Predictions. Neuroepidemiology. 2020;54(5):364-9.
Espíndola OM, Siqueira M, Soares CN, Lima M, Leite A, Araujo AQC, et al. Patients with COVID-19 and neurological manifestations show undetectable SARS-CoV-2 RNA levels in the cerebrospinal fluid. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2020;96:567-9.
Ellul M, Varatharaj A, Nicholson TR, Pollak TA, Thomas N, Easton A, et al. Defining causality in COVID-19 and neurological disorders. Journal of neurology, neurosurgery, and psychiatry. 2020;91(8):811-2.
Archie SR, Cucullo L. Cerebrovascular and Neurological Dysfunction under the Threat of COVID-19: Is There a Comorbid Role for Smoking and Vaping? International journal of molecular sciences. 2020;21(11).
Federico A. Brain Awareness Week, CoVID-19 infection and Neurological Sciences. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2020;41(4):747-8.
Medeiros KS, Ferreira de Paiva LM, Macêdo LTA, Farias de Souza W, Soares da Silva LA, Sarmento ACA, et al. Prevalence of Burnout Syndrome and other psychiatric disorders among health professionals during the COVID-19 pandemic: A systematic review and meta-analysis protocol. PloS one. 2021;16(12):e0260410.
Hoertel N, Sánchez-Rico M, Herrera-Morueco JJ, de la Muela P, Gulbins E, Kornhuber J, et al. Comorbid medical conditions are a key factor to understand the relationship between psychiatric disorders and COVID-19-related mortality: Results from 49,089 COVID-19 inpatients. Molecular psychiatry. 2021:1-3.
Gasnier M, Choucha W, Radiguer F, Bougarel A, Faulet T, Kondarjian C, et al. Acute Objective Severity of COVID-19 Infection and Psychiatric Disorders 4 Months After Hospitalization for COVID-19. The Journal of clinical psychiatry. 2021;83(1).
Looi JC, Allison S, Bastiampillai T, Pring W, Kisely SR. Telepsychiatry and face-to-face psychiatric consultations during the first year of the COVID-19 pandemic in Australia: patients being heard and seen. Australasian psychiatry : bulletin of Royal Australian and New Zealand College of Psychiatrists. 2021:10398562211046301.
Savilahti EM, Lintula S, Häkkinen L, Marttunen M, Granö N. Adolescent psychiatric outpatient care rapidly switched to remote visits during the COVID-19 pandemic. BMC psychiatry. 2021;21(1):586.
Oderinde KO, Akanni OO, Olashore A. Knowledge of the coronavirus disease 2019 (COVID-19) and sleep problems among a selected sample of psychiatric hospital staff in Nigeria: a cross-sectional study. The Pan African medical journal. 2021;40:39.
Vannorsdall TD, Brigham E, Fawzy A, Raju S, Gorgone A, Pletnikova A, et al. Rates of cognitive dysfunction, psychiatric distress and functional decline following COVID-19. Journal of the Academy of Consultation-Liaison Psychiatry. 2021.
Heilbronner U, Streit F, Vogl T, Senner F, Schaupp SK, Reich-Erkelenz D, et al. Interplay between the Genetics of Personality Traits, severe Psychiatric Disorders, and COVID-19 Host Genetics in the Susceptibility to SARS-CoV-2 Infection - ADDENDUM. BJPsych open. 2021;7(6):e206.
Duarte D, El-Hagrassy MM, Couto T, Gurgel W, Minuzzi L, Saperson K, et al. Challenges and Potential Solutions for Physician's Suicide risk factors in the COVID-19 Era: Psychiatric Comorbidities, Medicine Judicialization, and Burnout. Trends in psychiatry and psychotherapy. 2021.
Yang M, Feng Y, Yuan L, Zhao H, Gao S, Li Z. High Concentration and Frequent Application of Disinfection Increase the Detection of Methicillin-Resistant Staphylococcus aureus Infections in Psychiatric Hospitals During the COVID-19 Pandemic. Frontiers in medicine. 2021;8:722219.
Feeney A, Hock RS, Harmon HA, Caplin PS, Kobylski LA, Viguera AC, et al. Perinatal experiences of pregnant women with psychiatric disorders during the COVID-19 pandemic. General hospital psychiatry. 2021;73:114-9.
Januel D, Fourati T, Moulier V, Ledosseur Y, Bolloré O, Isaac C, et al. Prospective survey of psychiatric patients during the first confinement of the COVID 2019 pandemic. Asian journal of psychiatry. 2021;66:102888.
Min S, Jeong YH, Kim J, Koo JW, Ahn YM. The Aftermath: Post-pandemic Psychiatric Implications of the COVID-19 Pandemic, a South Korean Perspective. Frontiers in psychiatry. 2021;12:671722.
Amsalem D, Lazarov A, Markowitz JC, Naiman A, Smith TE, Dixon LB, et al. Psychiatric symptoms and moral injury among US healthcare workers in the COVID-19 era. BMC psychiatry. 2021;21(1):546.
Ahmed A, Chughtai NA. Psychiatric and post-traumatic stress disorders among COVID-19 survivors. Journal of emergency management (Weston, Mass). 2021;18(7):157-60.
Mistler LA, Auh E, Sanders E, Thomas J, Moore E, Fetter JC. Awake Proning for COVID-19 in a State Psychiatric Hospital: A Case Series. The primary care companion for CNS disorders. 2021;23(6).
Kazi SE, Akhter S, Periasamy D, Faruki F, Tahir R. Acute Psychosis and COVID-19 Infection: Psychiatric Symptoms in Hospitalized Patients. Cureus. 2021;13(9):e18121.
Fröhlich S, Imboden C, Iff S, Spörri J, Quednow BB, Scherr J, et al. Prevalence and Risk Factors of Psychiatric Symptoms among Swiss Elite Athletes during the First Lockdown of the COVID-19 Pandemic. International journal of environmental research and public health. 2021;18(20).
Dar SA, Dar MM, Sheikh S, Haq I, Azad A, Mushtaq M, et al. Psychiatric comorbidities among COVID-19 survivors in North India: A cross-sectional study. Journal of education and health promotion. 2021;10:309.
Albert H, Heipel D, Thakre TP, Hess O, Cooper K, Pryor R, et al. Management of the COVID-19-Infected Psychiatric Inpatients: Unique Infection Prevention Considerations and Evolving Strategies. Current treatment options in infectious diseases. 2021:1-10.
Truhan TE, Gianniou FM, Papageorgiou KA. Differences in psychiatric symptoms between the UK and Greece prior to and during COVID-19: The roles of subclinical narcissism and mental toughness. Personality and individual differences. 2022;185:111308.
Novick AM, Stoddard J, Johnson RL, Sammel MD, Berkowitz L, Epperson CN. Adapting psychiatric research in the age of COVID-19: role of online studies. BJPsych open. 2021;7(5):e177.
Dondé C, Pouchon A, Pelluet A, Bougerol T, Polosan M. The Impact of Wearing a Face Mask on the Psychiatric Interview: a National Survey During the COVID-19 Pandemic. The Psychiatric quarterly. 2021:1-8.
Saali A, Stanislawski ER, Kumar V, Chan C, Hurtado A, Pietrzak RH, et al. The Psychiatric Burden on Medical Students in New York City Entering Clinical Clerkships During the COVID-19 Pandemic. The Psychiatric quarterly. 2021:1-16.
Pompili M, Innamorati M, Sampogna G, Albert U, Carmassi C, Carrà G, et al. The impact of Covid-19 on unemployment across Italy: Consequences for those affected by psychiatric conditions. Journal of affective disorders. 2022;296:59-66.
Ren X, Shen F, Gui Y, Wang W, Xing B, Huang W. The attitudes of psychiatric patients towards COVID-19 vaccination in China: a cross-sectional study. BMC psychiatry. 2021;21(1):475.
Grover S, Sahoo S, Rijal R, Mehra A. Don't forget me in amidst of COVID-19 pandemic: A case series and review of literature on steroid associated psychiatric manifestations. Brain, behavior, & immunity - health. 2021;18:100345.
Smith TE, Rodgers IT, Silverman DJ, Dreslin SR, Olfson M, Dixon LB, et al. COVID-19 Case Rates After Surveillance and Vaccinations in a Statewide Psychiatric Hospital System. American journal of public health. 2021;111(10):1780-3.
Rømer TB, Christensen RHB, Blomberg SN, Folke F, Christensen HC, Benros ME. Psychiatric Admissions, Referrals, and Suicidal Behavior Before and During the COVID-19 Pandemic in Denmark: A Time-Trend Study. Acta psychiatrica Scandinavica. 2021;144(6):553-62.
Levitt G. COVID-19 Infection in an Inpatient Psychiatric Hospital Setting: Demographics, Outcomes, and Impact on Well-being. The primary care companion for CNS disorders. 2021;23(5).
Penninx B. Psychiatric symptoms and cognitive impairment in "Long COVID": the relevance of immunopsychiatry. World psychiatry : official journal of the World Psychiatric Association (WPA). 2021;20(3):357-8.
Schwartz AC, Brenner AM. Psychiatric Education and COVID-19: Challenges, Responses, and Future Directions. Academic psychiatry : the journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry. 2021;45(5):535-8.
Puangsri P, Jinanarong V, Wattanapisit A. Impacts on and Care of Psychiatric Patients during the Outbreak of COVID-19. Clinical practice and epidemiology in mental health : CP & EMH. 2021;17:52-60.
Zemlak JL, Wilson P, VanGraafeiland B, Rodney T. Telehealth and the Psychiatric Mental Health Nurse Practitioner: Beyond the COVID-19 Pandemic. Journal of the American Psychiatric Nurses Association. 2021:10783903211045119.
Yalçın M, Baş A, Bilici R, Özdemir Y, Beştepe EE, Kurnaz S, et al. Psychiatric emergency visit trends and characteristics in a mental health epicenter in Istanbul during COVID-19 lockdown. Social psychiatry and psychiatric epidemiology. 2021;56(12):2299-310.
Shen X, Koh MSH, Lim BY, Demo-Os M, Chien JMF, Santosa A, et al. Acute pericarditis and cardiac tamponade after Covid-19 vaccination. Singapore medical journal. 2021.
Duckheim M, Schreieck J. COVID-19 and Cardiac Arrhythmias. Hamostaseologie. 2021;41(5):372-8.
Akkawi AR, Ghazal M. COVID-19 and Cardiac Arrhythmias: A Review of the Literature. Cureus. 2021;13(9):e17797.
Fijałkowska J, Sobolewski J, Glińska A, Pisowodzka I, Nowak R, Żarczynska-Buchowiecka M, et al. Cardiac abnormalities detected by echocardiography and cardiac magnetic resonance in healthcare professionals recovered from non-severe COVID-19. Kardiologia polska. 2021;79(11):1256-8.
Breitbart P, Koch A, Schmidt M, Magedanz A, Lindhoff-Last E, Voigtländer T, et al. Clinical and cardiac magnetic resonance findings in post-COVID patients referred for suspected myocarditis. Clinical research in cardiology : official journal of the German Cardiac Society. 2021;110(11):1832-40.
Bloom CI, Johnston SL. Decline in respiratory and cardiac admissions during the COVID-19 pandemic: What is the role of common respiratory virus infections? Respirology (Carlton, Vic). 2021;26(11):1010-1.
Maddali MM, Munasinghe TD. A left Atrial Mass After COVID-19 and Cardiac Surgery. Journal of cardiothoracic and vascular anesthesia. 2021.
Erol N, Alpinar A, Erol C, Sari E, Alkan K. Intriguing new faces of Covid-19: persisting clinical symptoms and cardiac effects in children. Cardiology in the young. 2021:1-7.
Mohammed Sheata I, Smith SR, Kamel H, Varrassi G, Imani F, Dayani A, et al. Pulmonary Embolism and Cardiac Tamponade in Critical Care Patients with COVID-19; Telemedicine's Role in Developing Countries: Case Reports and Literature Review. Anesth Pain Med. 2021;11(2):e113752.
Huang Y, Hu Z, Hu D, Quan Z, Zhou X, Fan G, et al. Clinical characteristics, risk factors, and cardiac manifestations of cancer patients with COVID-19. Journal of applied physiology (Bethesda, Md : 1985). 2021;131(3):966-76.
Barssoum K, Victor V, Salem A, Kumar A, Mubasher M, Hassib M, et al. Echocardiography, lung ultrasound, and cardiac magnetic resonance findings in COVID-19: A systematic review. Echocardiography (Mount Kisco, NY). 2021;38(8):1365-404.
Cunningham JW, Claggett BL, Jering KS, Vaduganathan M, Bhatt AS, Rosenthal N, et al. Prognostic Value of Natriuretic Peptides and Cardiac Troponins in COVID-19. Circulation. 2021;144(2):177-9.
Calabrese M, Garofano M, Palumbo R, Di Pietro P, Izzo C, Damato A, et al. Exercise Training and Cardiac Rehabilitation in COVID-19 Patients with Cardiovascular Complications: State of Art. Life (Basel, Switzerland). 2021;11(3).
Grech N, Xuereb R, England K, Xuereb RG, Caruana M. When the patients stayed home: the impact of the COVID-19 pandemic on acute cardiac admissions and cardiac mortality in Malta. Zeitschrift fur Gesundheitswissenschaften = Journal of public health. 2021:1-7.
Vujaklija Brajković A, Zlopaša O, Gubarev Vrdoljak N, Goran T, Lovrić D, Radonić R. Acute liver and cardiac failure in multisystem inflammatory syndrome in adults after COVID-19. Clin Res Hepatol Gastroenterol. 2021;45(3):101678.
Talwar D, Kumar S, Acharya S, Khanna S, Hulkoti V. Paroxysmal Supraventricular Tachycardia and Cardiac Arrest: A Presentation of Pulmonary Embolism With Infarction as a Sequela of Long COVID Syndrome. Cureus. 2021;13(10):e18572.
Kim CW, Aronow WS. COVID-19, cardiovascular diseases and cardiac troponins. Future cardiology. 2021.
Diotallevi F, Mazzanti S, Properzi P, Olivieri S, Giacometti A, Offidani A. Is there a POST-COVID dermatological syndrome? The integrated dermato-infectious disease experience of a single centre. Journal of the European Academy of Dermatology and Venereology : JEADV. 2021.
Panda M, Dash S, Behera B, Sil A. Dermatological Manifestations Associated with COVID-19 Infection. Indian J Dermatol. 2021;66(3):237-45.
Jakhar D, Das A, Kaul S, Kaur I, Madke B, Dalal A. Prevalence and characteristics of dermatological manifestations in COVID-19 positive dermatologists: Report from a web-based survey in India. Journal of the European Academy of Dermatology and Venereology : JEADV. 2021;35(12):e832-e3.
Dowdle TS, Thompson M, Alkul M, Nguyen JM, Sturgeon ALE. COVID-19 and dermatological personal protective equipment considerations. Proceedings (Baylor University Medical Center). 2021;34(4):469-72.
Welsh EC, Alfaro Sanchez AB, Ortega Gutiérrez GL, Cardenas-de la Garza JA, Cuellar-Barboza A, Valdes-Espinosa RA, et al. COVID-19 dermatological manifestations: results from the Mexican Academy of Dermatology COVID-19 registry. Int J Dermatol. 2021;60(7):879-81.
González-Martín-Moro J, Guzmán-Almagro E, Izquierdo Rodríguez C, Fernández Hortelano A, Lozano Escobar I, Gómez Sanz F, et al. Impact of the COVID-19 Lockdown on Ophthalmological Assistance in the Emergency Department at a Spanish Primary Level Hospital. Journal of ophthalmology. 2021;2021:8023361.
Wasfy T, Eldesouky MA, Serag Y, Elbedewy HA. Concurrent and Post COVID-19 Ophthalmological Implications. Clinical ophthalmology (Auckland, NZ). 2021;15:4467-73.
Domínguez-Varela IA, Ortiz-Morales G, Gómez-Elizondo DE, Nava-García JA, Valdez-García JE. Ophthalmological Care Management of Cataract Patients During the COVID-19 Times: Perspectives From a Mexican Eye Health Care System. Asia-Pacific journal of ophthalmology (Philadelphia, Pa). 2021.
Khair D, Chaudhary V, Harissi-Dagher M. Success of the Canadian Ophthalmological Society's first virtual meeting amid COVID-19 pandemic. Canadian journal of ophthalmology Journal canadien d'ophtalmologie. 2021.
Schuh A, Kassumeh S, Schmelter V, Demberg L, Siedlecki J, Anschütz A, et al. Effects of the First COVID-19 Lockdown on Ophthalmological Patient Care. Klinische Monatsblatter fur Augenheilkunde. 2021;238(11):1220-8.
Magar ST, Gyawali BR. Otorhinolaryngological and Ophthalmological Manifestations of COVID-19 in the Pediatric Population. JNMA; journal of the Nepal Medical Association. 2020;58(232):1093-6.
France K, Glick M. Long COVID and oral health care considerations. Journal of the American Dental Association (1939). 2021.
Blum IR. Urgent dental care and oral health under the clouds of COVID-19. Primary dental journal. 2021;10(3):2.
Naqvi AR, Schwartz J, Brandini DA, Schaller S, Hussein H, Valverde A, et al. COVID-19 and oral diseases: Assessing manifestations of a new pathogen in oral infections. International reviews of immunology. 2021:1-15.
Riofrio G, Castillo S, Salcedo G, Alvitez-Temoche D, Watanabe R, Mayta-Tovalino F. Future Challenges of Covid-19 and Oral Manifestations in Daily Dental Practice: A Literature Review. Journal of International Society of Preventive & Community Dentistry. 2021;11(3):242-7.
Sharma A, Bhardwaj R. COVID-19 and ENT surgery: a brief review of essential precautions and triage. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2021;278(5):1301-5.
Herman P, Vincent C, Parietti Winkler C, Loundon N, Couloigner V, Tankere F, et al. Consensus statement. Corticosteroid therapy in ENT in the context of the COVID-19 pandemic. European annals of otorhinolaryngology, head and neck diseases. 2020;137(4):315-7.
Dave PK, Rojas-Cessa R, Dong Z, Umpaichitra V. Survey of Saliva Components and Virus Sensors for Prevention of COVID-19 and Infectious Diseases. Biosensors. 2020;11(1).
Alamoodi AH, Zaidan BB, Zaidan AA, Albahri OS, Mohammed KI, Malik RQ, et al. Sentiment analysis and its applications in fighting COVID-19 and infectious diseases: A systematic review. Expert systems with applications. 2021;167:114155.
Agarwal D, Saxena R, Sinha R, Mishra D, Sachdev MS, Sharma N. All India Ophthalmological Society Financial Impact Survey on ophthalmology practice in India during COVID-19. Indian journal of ophthalmology. 2021;69(8):2196-201.
Khan SI, Versha F, Bai P, Bachani P, Nawaz MU, Kumar L, et al. Frequency of Ophthalmological Findings in Hospitalized COVID-19 Patients. Cureus. 2021;13(5):e14942.
Pandey N, Kumar S, Kesar SD, Dandu HR, Ankita, Maurya VK, et al. An Ophthalmological update for air-travellers during COVID-19. Travel medicine and infectious disease. 2021;39:101955.
Gandhi A, Naik M, Narula A. Ophthalmological manifestations of COVID-19 and its transmissibility via ocular route. Postgraduate medical journal. 2021;97(1147):329.
Pellegrini M, Roda M, Lupardi E, Di Geronimo N, Giannaccare G, Schiavi C. The impact of COVID-19 pandemic on ophthalmological emergency department visits. Acta ophthalmologica. 2020;98(8):e1058-e9.
Vargas-Peirano M, Navarrete P, Díaz T, Iglesias G, Hoehmann M. Care of ophthalmological patients during the COVID-19 pandemic: A rapid scoping review. Medwave. 2020;20(4):e7902.
Giannaccare G, Buzzi M, Versura P. Use of eye drops obtained from homologous blood source in the time of COVID-19: is there cause for ophthalmological concern? Blood transfusion = Trasfusione del sangue. 2020;18(3):233-4.
Siedlecki J, Brantl V, Schworm B, Mayer WJ, Gerhardt M, Michalakis S, et al. COVID-19: Ophthalmological Aspects of the SARS-CoV 2 Global Pandemic. Klinische Monatsblatter fur Augenheilkunde. 2020;237(5):675-80.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Since making research freely available supports a greater global exchange of knowledge, PreferPub provides immediate open access to its published books under the terms of the Creative Commons Attribution-NonCommercial 4.0 License (CC BY-NC 4.0). This license allows others to share, copy, and redistribute the material in any medium or format, as well as adapt, remix, transform, and build upon the material, as long as the use is non-commercial and appropriate credit is given to the original work.




